ENTIRE CLASS:
NR548 – Psychiatric Assessment for Psychiatric-Mental Health Nurse Practitioner
NR548 Week 4: Psychiatric History Assignment Video and Documentation
General Instructions
This assignment has two components: a recorded presentation via Kaltura and written psychiatric history.
- Create a recording for educational purposes per the assignment guidelines. This video will be viewed by your instructor and other Chamberlain officials as needed for educational and related purposes. This video will not be posted for public viewing. Use the following guidelines:
- Select a volunteer participant, age 13 or older, to demonstrate the psychiatric history assignment. If the volunteer is a minor, you must be the parent or guardian.
- Select a private environment without background noises or distractions where you will be able to conduct the interview.
- You are permitted to have a sheet of paper with interview assessment headings listed to facilitate the interview; you may not use textbooks, notes, or other assistive materials.
- State in front of the camera: “My name is [First and Last Name of Student] and this is my psychiatric history interview for NR 548.”
- Ask the participant to state in front of the camera: “My name is [First and Last Name of Adult Participant] and I give my permission for this interview to be recorded and submitted to Chamberlain College of Nursing for grading purposes.”
- If the volunteer is a minor, you must be their parent/guardian and provide consent. “I am the parent/guardian of [First and Last Name of Minor Participant] and I give my permission for this interview to be recorded and submitted to Chamberlain College of Nursing for grading purposes.”
Required components
Include the following information in the recorded interview and in the written psychiatric history template..
- History of present illness (HPI)
-
- Include the chief complaint in quotation marks
- List only HPI data
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow.
- Medications
-
- Provide all current medication information
- Include all criteria from the medication table
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow.
- Past psychiatric history
-
- Include entire past psychiatric history
- Address all criteria listed on the template
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow
- Medical history
-
- Include all relevant medical information
- Address all criteria listed on the template
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow
- Family history
-
- Include all pertinent family history
- Address all criteria listed on the template
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow
- Social history
-
- Include all relevant information from the social history
- Address all criteria listed on the template
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow
- Review of systems
-
- Include a complete review of systems
- Address all criteria listed on the template
- Use appropriate terminology
- Provide information that is understandable, well-organized, and easy to follow
- Formatting
-
- Use provided template
- Use correct grammar, spelling, and punctuation
- Use consistent font throughout the template
SOLUTION
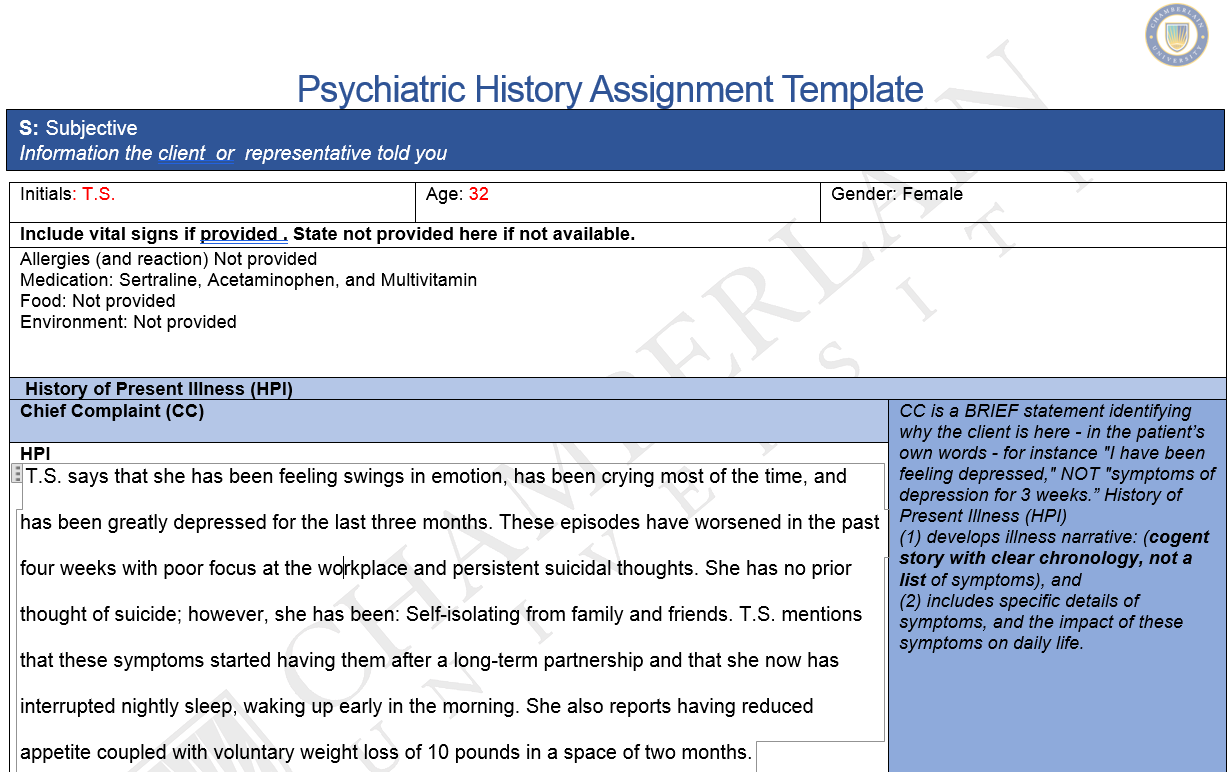
| S: Subjective
Information the client or representative told you |
Psychiatric History Assignment Template
| Initials: T.S. | Age: 32 | Gender: Female | |
| Include vital signs if provided . State not provided here if not available. | |||
| Allergies (and reaction) Not provided
Medication: Sertraline, Acetaminophen, and Multivitamin Food: Not provided Environment: Not provided |
|||
| History of Present Illness (HPI) | |||
| Chief Complaint (CC)
|
CC is a BRIEF statement identifying why the client is here – in the patient’s own words – for instance “I have been feeling depressed,” NOT “symptoms of depression for 3 weeks.” History of Present Illness (HPI)
(1) develops illness narrative: (cogent story with clear chronology, not a list of symptoms), and (2) includes specific details of symptoms, and the impact of these symptoms on daily life.
|
||
| HPI
T.S. says that she has been feeling swings in emotion, has been crying most of the time, and has been greatly depressed for the last three months. These episodes have worsened in the past four weeks with poor focus at the workplace and persistent suicidal thoughts. She has no prior thought of suicide; however, she has been: Self-isolating from family and friends. T.S. mentions that these symptoms started having them after a long-term partnership and that she now has interrupted nightly sleep, waking up early in the morning. She also reports having reduced appetite coupled with voluntary weight loss of 10 pounds in a space of two months.
|
|||
……………………………….purchase solution at $10 only

Reviews
There are no reviews yet.